UC HEALTH LINE: Women Should Speak With Physician About HPV Concerns
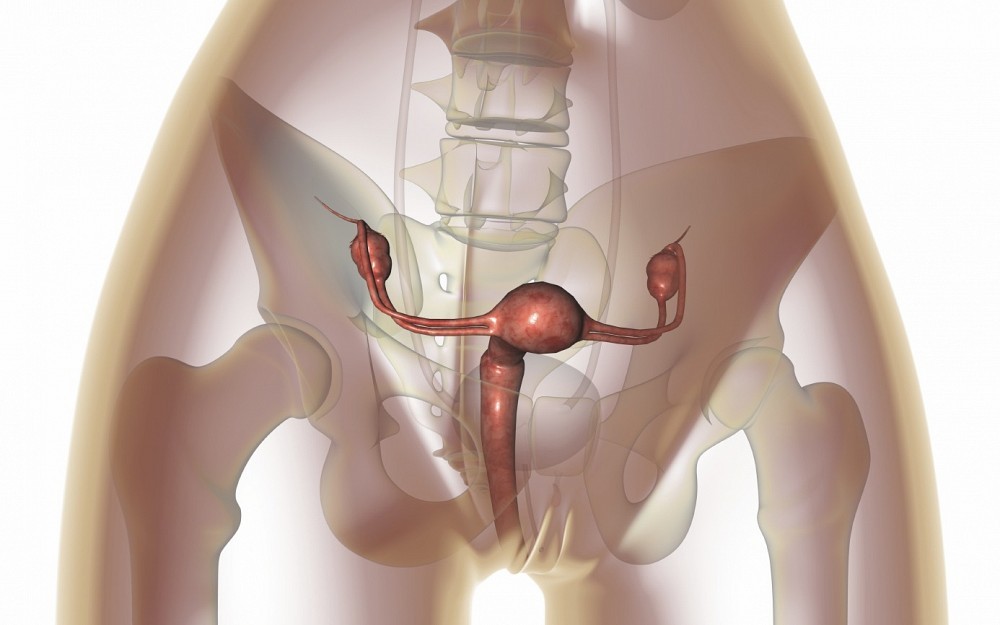
CINCINNATIIts Cervical Cancer Screening Month, and womens health professionals suggest that women of all ages educate themselves about the human papillomavirus (HPV), known to be present in most all cervical cancers.
According to the U.S. Centers for Disease Control and Prevention, HPV is a very common virus found mostly in women and can be sexually transmitted. There are approximately 150 forms of the virus, and more than 40 HPV types can infect the genital areas of males and females. HPV infection is most common in people in their late teens and early 20s.
"Not every woman who tests positive for HPV is going to develop cervical cancer, but there are some who will and its important to know whether you have HPV or not and monitor your health if you do, says Amy Thompson, MD, a UC Health gynecologist and assistant professor of obstetrics and gynecology at the University of Cincinnati (UC) College of Medicine.
While the CDC estimates that 12,000 women each year are diagnosed with cervical cancer and 4,000 women die from this disease in the U.S., Thompson says a woman may not even realize she has HPV unless she develops symptoms or undergoes a test performed by her doctor. Transmission, she says, can include skin to skin contact as occurs during hand/genital, oral/genital, or genital/genital touching and condoms do not prevent transmission.
One visual symptom of HPV is the development of genital warts. This condition is caused by the types of HPV that are less likely to cause cervical cancer. Genital warts can be painful and embarrassing, but there are treatments such as topical medications and office procedures to remove them. Other sexually transmitted types of HPV do not appear to cause cancer and are called low-risk HPVs.
In many cases HPV clears up on its own and does not cause any further damage, but sometimes HPV infections can persist for many years. Persistent infections with high-risk, or carcinogenic HPVs, are the primary cause of cervical cancer and anal cancer. HPV infections also cause some cancers of the vulva, and vagina.
The Food and Drug Administration (FDA) has approved two vaccines that are highly effective in preventing persistent infections with the two HPV types that cause most cervical and anal cancers. One of the vaccines also prevents infection with the two HPV types that cause most genital warts.
Thompson stresses that HPV is not the same as herpes or HIV (the virus that causes AIDS). These are all viruses that can be passed on during sex, but they cause different symptoms and health problems.
"It is important to speak with your physician about the HPV tests and the vaccines, Thompson says.
To make an appointment with Amy Thompson, MD, or another UC Health OBGYN provider, call 513-475-8588.
Related Stories
Celebrating all things Cincinnati
May 21, 2024
Hoxworth Blood Center announces the sixth annual Cincinnati Favorites Blood Drive Tour.
Does CBD really work?
May 21, 2024
The University of Cincinnati's LaTrice Montgomery and Michael Privitera joined WVXU's Cincinnati Edition to discuss how claims about CBD measure up to scientific research.
UC study uses health factors to predict kidney function recovery
May 21, 2024
Researchers at the University of Cincinnati College of Medicine have created a scoring model that uses key health indicators to accurately predict recovery for patients who suffer kidney failure due to acute kidney injury (AKI).
