Research Shows Potential Benefit of Integrative Medicine Practices
New research from the University of Cincinnati (UC) Center for Integrative Health and Wellness shows how integrative practices may help improve resiliency in medical students and reduce symptoms of patients undergoing cancer treatment.
UC medical students Emily Moss and Ellen Drosnick will present two abstracts of pilot studies in highlighted poster sessions at the 2018 International Congress on Integrative Medicine and Health, May 8-11, in Baltimore.
Sian Cotton, PhD, professor in the Department of Family and Community Medicine at the UC College of Medicine and director of both the UC Center for Integrative Health and Wellness and UC Health Integrative Medicine, is the senior author on both abstracts.
"Both of these pilot studies highlight the continued need for attention to the promotion of wellness and reduction of suffering for both community members facing cancer and students training in oftentimes stressful environments, Cotton says. Moss is principal investigator on the resiliency study, and Drosnick is principal investigator on the cancer study.
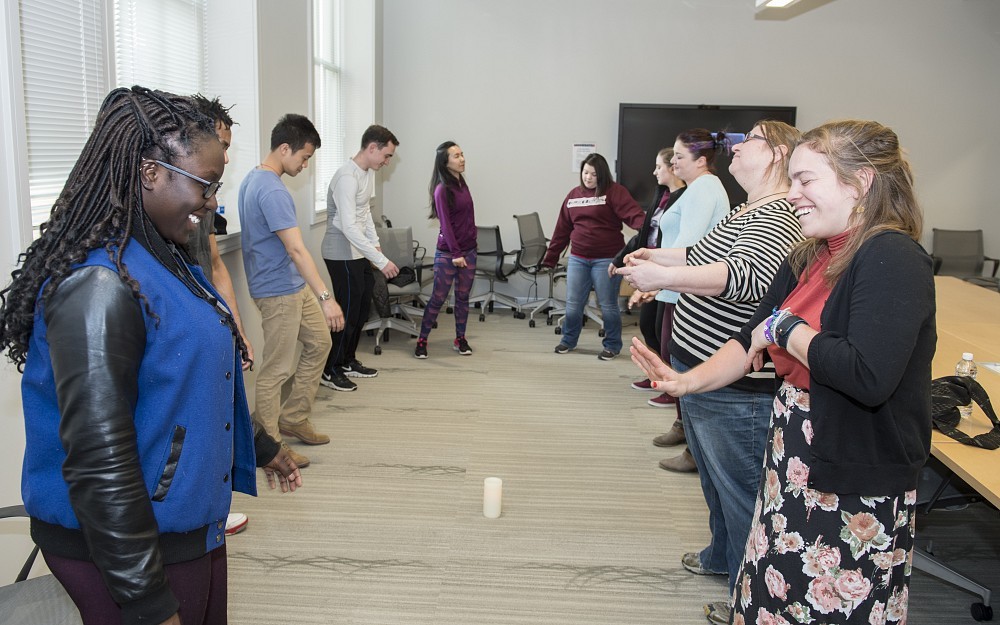
Resiliency in Medical Students
"Increasing resiliency in medical students is a key factor in promoting wellness during the rigors of medical school, says Cotton. "The purpose of this study was to examine mental and emotional factors related to resiliency as a target for future resiliency programming.
As part of the study, researchers provided an online survey to incoming students (178) and medical students in their first, second and third years of training at the UC College of Medicine (505). They were assessed on their feelings of stress, resiliency, mindfulness, empathy, burnout and a number of other of other factors, like anxiety, sleep disturbance, depression and fatigue. They were categorized into low versus high resiliency and compared among years using an approved analysis tools.
"Of the 683 students who completed the survey, students who were categorized as having high resiliency (80 percent) across all years scored better on most measures as compared to their low resiliency peers, she says. "Higher mindfulness, more positive affect, less stress and less anxiety were associated with higher resiliency. In qualitative responses, students identified creating a plan and gaining perspective as key to improved resiliency. Students reported that their resiliency could be increased with more free time, mentorship and better access to wellness resources at school.
"Resilience in these medical students was related to increased mindfulness and better mental health. Most students reported high levels of personal resiliency and identified feasible targets for school enhancement of resiliency. We believe that developing resiliency programs that emphasize mindfulness while reducing stress of medical students should be prioritized in medical schools. This is a relatively small sample size and more studies are needed to confirm these data as well as help us gain further knowledge of the effect of mind-body practices and other wellness interventions on medical student populations.
Mind-Body Practices Delivered in a Cancer Infusion Suite to Reduce Symptoms and Improve Well-Being for Patients
"Anxiety, pain, nausea and fatigue are common side effects of patients undergoing chemotherapy. Mind-body practices, like yoga therapy, breathing exercises, mindful awareness and auricular, or ear, acupuncture, have been shown to be effective in reducing symptoms in outpatient settings, Cotton says. "The purpose of this practice-based study was to assess the use of mind-body practices delivered at the point of care during chemotherapy infusion and to examine changes in symptoms before and after the intervention.
In this study, two mind-body practitioners delivered services within a cancer infusion suite. Patients were asked if they were interested in experiencing a mind-body practice while in the infusion suite, to help with symptom reduction. A variety of mind-body practices, including breathwork, guided imagery and mindfulness practices, were used depending on patient preference and practitioner expertise, and a pre- and post-intervention brief survey was collected, documenting patients ratings of symptomspain, nausea, fatigue, anxiety and overall distresson a scale from 0 to 10 (none to unbearable). Data were also collected to document unprompted patient feedback related to the intervention.
"Of the 191 patients, with various cancers and blood disorders, who participated in this study from April 2016 to July 2017, 86 percent (165 patients) participated and completed both pre- and post-surveys. Levels of anxiety (3.61 pre vs. 1.73 post), pain (1.82 pre vs. 1.02 post), nausea (.72 pre vs. .326 post) and overall distress (3.48 pre vs. 1.83 post) all significantly decreased post intervention. Additionally, 32 percent of participants (22 patients) spontaneously reported that the treatment was relaxing and/or soothing.
"In this study, clinical symptoms were shown to decrease following a mind-body intervention in a cancer infusion suite delivered at the point of care. Future studies should use objective raters to assess symptom reduction and should include a larger sample size; however, this preliminary study shows that mind-body practices delivered during infusion services may provide symptom reduction for patients and should be rigorously assessed for dose, individualized preference and long-term symptom improvement.
For more information on the UC Center for Integrative Health and Wellness activities, please visit https://med.uc.edu/integrative.
Related Stories
Local 12: Head injury survivor, doctor share importance of...
April 23, 2024
Local 12 spoke with patient Shane Shapiro and the University of Cincinnati's Laura Ngwenya about the importance of wearing a helmet following Shapiro's traumatic brain injury and recovery.
UC hires Dr. Gregory Postel as senior vice president of health...
April 23, 2024
UC Board of Trustees vote to hire Dr. Gregory Postel as senior vice president of health affairs and dean of UC College of Medicine.
Hoxworth Blood Center's Research Division shines with 2023...
April 22, 2024
Hoxworth Blood Center's Research Division Shines with 2023 National and International Publications: A Milestone Year in Transfusion Medicine.
