UC experts present research at International Stroke Conference 2026
Abstracts examine post-stroke symptoms and swallowing issues, increased incidence in young adults
University of Cincinnati researchers are presenting research at the International Stroke Conference 2026 in New Orleans Feb. 4-6.
Specific symptoms associated with varying disability outcomes following stroke

Paul Wechsler, MD. Photo/University of Cincinnati.
Patients can have a variety of symptoms when experiencing an ischemic stroke, caused by a clot blocking a blood vessel in the brain. Doctors choose whether to treat the stroke with clot-busting medication or to remove the blood clot mechanically, in part by determining if stroke symptoms may lead to long-term disability where a patient is dependent on others because they are not able to carry out daily living activities.
“However, doctors often struggle to know at the time of stroke treatment decision-making if the symptoms a person is having may be disabling in the future,” said Paul Wechsler, MD, assistant professor in the Department of Neurology and Rehabilitation Medicine in UC’s College of Medicine and a UC Gardner Neuroscience Institute stroke physician. “We asked the question: what symptoms and neurologic deficits patients have at stroke presentation lead to disability three months after a stroke?”
Wechsler and colleagues found patients who have difficulty walking or leg weakness are more likely to be disabled or die three months following the stroke. Patients with numbness following a stroke are less likely to be disabled or die three months after a stroke.
“We hope this information will help doctors decide which stroke patients should receive clot-busting medications or the procedure to mechanically remove the blood clot, as these procedures have inherent risks that may not be worth taking for all stroke patients,” Wechsler said. “Further research is needed to determine the symptoms and neurologic deficits that may lead to poor quality of life in stroke patients, as we know physical functioning is only one aspect that contributes to people's quality of life.”
Wechsler will present “Symptoms and neurologic deficits at stroke presentation associated with functional dependence and health-related quality of life after minor acute ischemic stroke” Feb. 4 at 12:30 p.m.
Study identifies ‘silent’ swallowing problems after stroke

Brittany Krekeler, PhD. Photo/Rachel Treinen Photography.
Up to three-quarters of all stroke survivors have some form of difficulty swallowing (dysphagia) after a stroke, but the problems cannot be addressed if they go unnoticed.
Brittany Krekeler, PhD, and colleagues studied whether stroke survivors continue to have swallowing difficulties even if they don’t feel or report any symptoms.
“We also examined whether common questionnaires patients complete about swallowing actually reflect what is happening in the throat when swallowing is directly observed using imaging of someone’s swallowing, which is an X-ray video called a swallow study,” said Krekeler, associate professor and clinician-scientist at the UC College of Medicine’s Dysphagia Rehabilitation Laboratory.
The team found approximately one out of every six stroke survivors participating in studies had “silent swallowing problems,” meaning they had real difficulty protecting their airway or clearing food and liquid without reporting the feeling of any swallowing trouble.
“Importantly, these individuals had swallowing impairments that were just as severe as those who did report symptoms,” Krekeler said. “This shows that feeling ‘fine’ does not always mean swallowing is safe, and relying only on patient-reported symptoms may cause clinicians to miss people who are at risk for complications like pneumonia, dehydration or poor nutrition.”
Moving forward, the team is focusing on tracking swallowing recovery over time after a stroke, particularly in people whose swallowing problems are silent and easily missed. The long-term goals are to determine who is most at risk, when follow-up swallowing evaluations should occur and how to best prevent avoidable complications.
Krekeler will present the digital oral abstract “Silent Dysphagia After Stroke: Prevalence, Risk Factors, and Clinical Implications from a Pilot Cohort Study” Feb. 4 at 3:39 p.m.
Population study reveals increased stroke incidence in younger adults

Emily Fisher, MD. Photo/University of Cincinnati.
Previous research has suggested that rates of death after stroke for younger adults are rising.
Researchers, including abstract first author Emily Fisher, MD, examined data from the Greater Cincinnati Northern Kentucky Stroke Study to calculate how many young people are having strokes in the area and determine their short-term mortality rates over time.
The team found that the incidence of stroke in young adults (aged 54 and younger) is rising over time, but short-term mortality rates for this group are decreasing. Stroke incidence in adults 55 and up is declining.
“This work highlights the need for continued study of young adults with stroke,” said Fisher, a vascular neurology fellow in the Department of Neurology and Rehabilitation Medicine in UC’s College of Medicine. “Young adults with stroke often have different reasons for their strokes compared to older adults, and so it's important to learn more about this age group.”
Fisher will present “Temporal Trends in the Incidence and Case Fatality Rates of Stroke in the Young: A Population-Based Study” Feb. 4 at 7:40 a.m.
Blood fat levels tied to patient recovery after intracerebral hemorrhage

Aysegul Gezer, DO. Photo/University of Cincinnati.
Only approximately 25% of survivors regain independence following an intracerebral hemorrhage (ICH), and researchers are focusing on how recovery and secondary injury following the stroke affect long-term outcomes.
A team that includes first author Aysegul Gezer focused on how certain fats in the blood, called sphingolipids, are linked to patient recovery after ICH.
“In particular, we asked whether differences in these molecules could help explain why some patients recover independence while others do not, and whether this relationship differs depending on where the brain bleed occurs,” said Gezer, DO, a vascular neurology fellow in the Department of Neurology and Rehabilitation Medicine in UC’s College of Medicine.
The team analyzed 48 plasma samples from patients after ICH and found no sphingolipid differences in patients with good outcomes. Patients with worse recovery outcomes had distinct changes in sphingolipid levels, specifically around a molecule called sphingosine-1-phosphate (S1P).
“S1P is known to affect inflammation, blood vessel integrity and brain swelling,” Gezer said. “Importantly, these changes looked different depending on the location of the hemorrhage (deep versus. lobar regions of the brain). This suggests that the biological processes driving recovery may not be the same for all types of brain bleeds.”
Moving forward, the team will examine a larger patient cohort to confirm whether these blood markers can help predict recovery or guide treatment decisions. S1P-targeting medications are already used for other neurologic diseases, so that could eventually be an avenue to improve outcomes for ICH patients.
“This study helps move the field toward a more biologically personalized approach to brain hemorrhage and recognizing that stroke recovery is influenced not only by bleed size and location, but also by the body’s molecular response to injury,” Gezer said. “We need to do more hard work before implementing these findings clinically.”
Gezer will present “Alterations in Sphingolipid Pathway Associate with Clinical Outcomes After Intracerebral Hemorrhage” Feb. 4 at 12:30 p.m.
Acute anemia after stroke associated with worse white matter connectivity
Patients can experience acute anemia, a rapid drop in hemoglobin levels, after an intracerebral hemorrhage. Gezer and colleagues asked if this acute anemia is associated with damage to white matter, the brain’s communication pathways that allow different brain regions to talk to one another.
The researchers found patients with a greater drop in hemoglobin during hospitalization showed worse white matter connectivity on MRI scans, even in parts of the brain not directly affected by the initial bleed.
“Interestingly, a patient’s hemoglobin level when they first arrived at the hospital did not show this relationship,” Gezer said. “This implicates that it was the change over time that mattered most.”
With this preliminary data, the team will now explore whether anemia-related white matter injury contributes to long-term cognitive or physical disability and if treating or preventing anemia after ICH protects the brain and improves recovery.
“This work suggests that anemia after stroke may be more than just a lab abnormality, and it may represent a modifiable factor that affects brain health and recovery, opening the door to new supportive care strategies in stroke patients,” Gezer said.
Gezer will present “Acute Anemia After Intracerebral Hemorrhage Associates with Impaired White Matter Connectivity” Feb. 5 at 12:30 p.m.
Population study examines stroke recurrence rates

David Robinson, MD. Photo/University of Cincinnati.
Approximately a quarter of all strokes occur in people who have already experienced a prior stroke. Known as recurrent strokes, these secondary events present higher risks of death and disability compared to an initial stroke.
Recurrent strokes are common among all populations, but previous data showed they are more likely to occur among Black individuals.
Researchers led by David Robinson, MD, examined data from the Greater Cincinnati Northern Kentucky Stroke Study to see if there had been any changes in stroke recurrence between 2015 and 2020. The long-running study’s data is a representative sample of the entire United States and includes data from a range of care settings, including community hospitals and academic health centers.
A close examination of the data revealed white individuals experienced a decline in stroke recurrence between 2015 and 2020, while Black patients had a stable to increased recurrence risk over that time.
Robinson said exact reasons for this pattern are unclear, but research next steps include focusing on how stroke secondary prevention (the medications and lifestyle changes doctors recommend after an initial stroke) is implemented across the country.
“There also may be opportunities to reduce the burden of recurrence through implementation of new electronic medical record-based tools to facilitate consistent evidence-based secondary prevention regardless of care setting,” said Robinson, assistant professor in the Department of Neurology and Rehabilitation Medicine in UC’s College of Medicine.
Robinson will present “Evidence of widening racial disparities in stroke recurrence from 2015 to 2020: A population-based study” Feb. 5 at 3:15 p.m.
Study gives overview of current stroke telemedicine efforts in Latin America and Caribbean

Nathaly Chinchihualpa, MD. Photo/University of Cincinnati.
Like their colleagues from other specialties since the COVID-19 pandemic, stroke researchers are studying the feasibility and effectiveness of telemedicine-based care.
Led by Nathaly Chinchihualpa, MD, researchers examined how telemedicine-based stroke care has been implemented in Latin America and the Caribbean.
“Our review found that telemedicine for stroke care is feasible and widely implemented across countries in Latin America and the Caribbean, particularly through telestroke networks,” said Chinchihualpa, a research fellow in the Department of Neurology and Rehabilitation Medicine in UC’s College of Medicine. “Most studies reported comparable clinical performance to in-person care, along with shorter treatment times and improved continuity of care, especially in urban settings.”
The review was limited by the evidence being mostly observational and heterogeneous, and by data available from rural settings.
“This work provides a regional overview of real-world telemedicine use in stroke care and highlights the need to focus on prospective and comparative studies, standardized outcomes, longer follow-up and greater inclusion of rural and resource-limited settings in the region,” Chinchihualpa said. “Further work on cost-effectiveness and implementation strategies will also be valuable to support health system planning and policy development in the region.”
Chinchihualpa will present “Impact of Telemedicine for Stroke Care in Latin America and the Caribbean: A Systematic Review” Feb. 4 at 12:30 p.m.
Study: Early post-stroke seizure rates have not changed over time

Monica Sarkar, MD. Photo/University of Cincinnati.
Post-stroke epilepsy is a major contributor to rising rates of epilepsy among older individuals.
Early post-stroke seizures occur within the first seven days after a stroke and are the most common cause of new-onset epilepsy in older adults. Prior to this study, it was unknown whether rates of these seizures have changed due to the increased use of treatments that help restore blood flow to the brain.
Led by Monica Sarkar, MD, researchers reviewed data from 2005 to 2020 to examine the prevalence and trends of early post-stroke seizures.
“Interestingly, the incidence of early post-stroke seizures remained stable from 2005 to 2020,” said Sarkar, a fellow in the Department of Neurology and Rehabilitation Medicine in UC’s College of Medicine. “Hemorrhagic stroke has the highest risk of early post-stroke seizures.”
Patients with ischemic stroke complicated by bleeding, also known as ischemic stroke with hemorrhagic transformation, had the next-highest risk of early post-stroke seizure. Overall, incidences of ischemic stroke with hemorrhagic transformation have increased over time.
Next, the team is looking at three-year hospital admission rates for post-stroke seizure to learn more about specific risk factors of post-stroke epilepsy.
Sarkar will present “Rate of Early Post-Stroke Seizures Has Not Changed Over Time: A Population-Based Study” Feb. 4 at 4:57 p.m.
Ongoing trials
UC researchers will also present poster updates on several ongoing clinical trials, including:
- SISTER, a trial testing the efficacy of a new monoclonal antibody to treat acute ischemic stroke patients up to 24 hours after symptom onset. Eva Mistry, MBBS, will present “Strategy for Improving Stroke Treatment Response (SISTER): A Phase-2 Clinical Trial of TS23, a novel mechanism for improving outcomes in acute ischemic stroke” Feb. 5 at 12:30 p.m.
- TESTED, a trial examining the effectiveness of a stroke treatment for patients with a pre-stroke disability, one of the first studies to focus on this population. Mistry will present “Treatment with Endovascular Intervention for Stroke Patients with Existing Disability (TESTED): A Comparative Effectiveness Study” Feb. 5 at 12:30 p.m.
- STEP, the first-ever platform trial for acute ischemic stroke. Mistry will present “NIH StrokeNet Thrombectomy Endovascular Platform (STEP) Trial” Feb. 5 at 12:30 p.m
- ARPEGGIO, a trial testing an experimental drug to protect injured brain cells for patients with acute ischemic stroke. Mistry will present “ARPEGGIO Phase 2 Trial of Scp776, a First-in-Class Cerebroprotective Agent in Patients Undergoing Endovascular Thrombectomy: Pre-Specified Efficacy Analyses” Feb. 5 at 5:10 p.m.
Innovation Lives Here
The University of Cincinnati is classified as a Research 1 institution by the Carnegie Commission and is ranked in the National Science Foundation's Top-35 public research universities. UC's medical, graduate and undergraduate students and faculty investigate problems and innovate solutions with real-world impact.
Other UC involvement at ISC includes:
Chinchihualpa presenting “Burden of Stroke Across Altitude Gradients in Peru: A Nationwide Ecological Analysis, 2020-2024” Feb. 4 at 12:30 p.m.
Nejla Ghane, MD, presenting “Association of Infection with 3- and 6-Month Outcomes After Intracerebral Hemorrhage” Feb. 4 at 12:30 p.m.
Hyacinth I. Hyacinth, MD, PhD, presenting the invited symposium “Sickle Cell and Vascular Disease” Feb. 4 at 2:42 p.m.
Broderick presenting the poster “NIH StrokeNet” Feb. 5 at 12:30 p.m.
Mistry receiving the American Heart Association Stroke Council’s Mid-Career Achievement Award
Former UC faculty member Pooja Khatri, now at Yale University, receiving the AHA’s William M. Feinberg Award for Excellence in Clinical Stroke
Ronald Lazar, MD, of the University of Alabama at Birmingham presenting findings from the CREST-2 trial Feb. 4 at 12:09 p.m. As the NIH StrokeNet National Coordinating Center, UC researchers served as the central institutional review board for this trial.
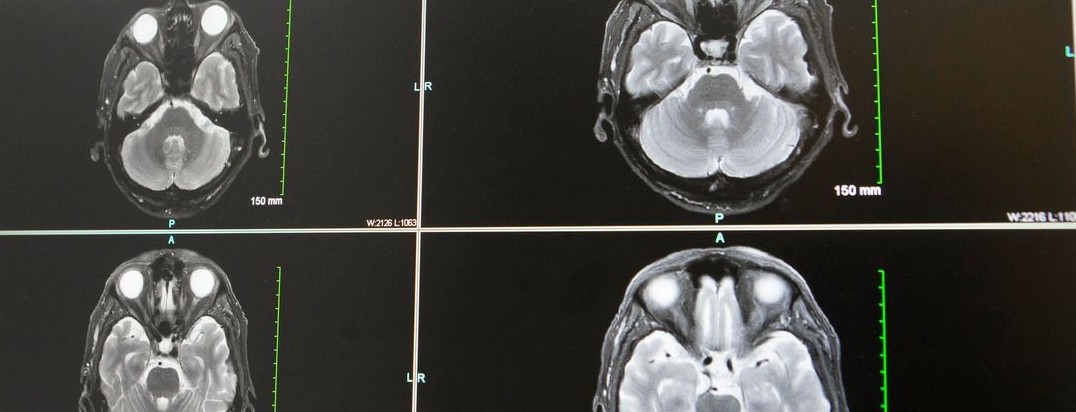
Featured photo at top of brain scans. Photo provided by Joseph Broderick.
Related Stories
A potential new treatment for brain tumors
September 23, 2022
The University of Cincinnati's Pankaj Desai, PhD, has received a $1.19 million grant from the National Institutes of Health/National Institute of Neurological Disorders and Stroke to continue research into the use of a drug called letrozole to treat glioblastomas, the most deadly form of brain tumors.
Collaborative University of Cincinnati Cancer Center team opens Phase 2 brain tumor trial
March 26, 2024
A multidisciplinary team of University of Cincinnati Cancer Center researchers have opened a Phase 2 clinical trial to test a new combination treatment for glioblastomas, the most deadly form of brain tumors.
UC trial tests tongue exercises to improve swallowing function after stroke
January 9, 2024
A new trial at the University of Cincinnati Gardner Neuroscience Institute, funded by a $660,000 National Institutes of Health (NIH) grant, will test an at-home tongue endurance exercise to improve patients’ swallowing function after a stroke.
