UC study: Protein helps prevent breast cancer metastasis
Novel findings of systematic study published in Cell Reports
While better screening and improved treatments are leading to better outcomes for patients with breast cancer, 90% of breast cancer deaths are a result of metastasis, or the cancer growing and spreading to other parts of the body.
University of Cincinnati Cancer Center researchers in the lab of Jun-Lin Guan, PhD, have identified a new protein that helps prevent metastasis of a subset called HER2-positive breast cancer. About 20% of patients have HER2-positive breast cancer, and these cancers tend to be more aggressive than other types.
The study findings were recently published in the journal Cell Reports.
Study background

Mingang Hao, PhD. Photo provided.
Guan’s lab has focused on how autophagy, or the cell's “recycling” function, affects cancer metastasis.
“Autophagy can be likened to a self-cleansing mechanism within cells,” said Mingang Hao, PhD, first author of the study and research scientist in Guan’s lab. “It allows them to eliminate undesirable or harmful components and emerge stronger and unharmed. In the context of cancer, dysfunctional autophagy has been linked to the development and progression of tumors.”
Research published in 2021 led by Hao found that blocking autophagy in HER2-positive breast cancer cells helped eliminate cancer development in an animal model of the disease. However, it was not clear whether the autophagy blockade also inhibited the process of cancer metastasis, as the lack of metastasis could be due to the elimination of the primary tumor growth in the model.
Very few studies in the field have directly examined the role of autophagy in metastasis, and most studies focused on genes thought to only play a role in autophagy (so-called “core” autophagy genes).
“In addition to these primary autophagy genes, which have been a major focus of research on cancer development and progression, there are many other proteins which regulate autophagy within cells,” Hao said.
I view this as one of the most important findings from my lab and a culmination of a lot of research expertise.
Jun-Lin Guan, PhD
Study results
Using CRISPR gene-editing technology, Hao and his colleagues created a specialized genetic library that targeted 171 different genes that are involved in autophagy regulation. By “turning off” each gene, the researchers aimed to identify specific genes that prevented the spread of breast cancer cells.
Using this technique, Hao said they identified a protein called p47 that prevents breast cancer metastasis.
“It does this by affecting different cellular pathways that are crucial for tumor cell movement,” Hao said. “These findings help us better understand the mechanisms behind cancer metastasis and may eventually lead to new strategies for preventing or treating the spread of breast cancer.”
In human breast cancer samples, lower p47 expression was correlated with higher breast cancer metastasis.
“This is one of the first few studies that links a particular autophagy regulatory gene with cancer metastasis with clear mechanisms that can potentially lead to the development of new therapies,” said Guan, professor and former chair of the Department of Cancer Biology in UC’s College of Medicine. “I view this as one of the most important findings from my lab and a culmination of a lot of research expertise as well as unique reagents we generated over the years.”

Jun-Lin Guan, PhD. Photo/Colleen Kelley/UC Marketing + Brand.
Guan said cancer drugs are often developed to inhibit a gene that helps cancer cells grow, but in the case of p47, a potential therapy would seek to increase the functions of the protein so that it can prevent metastasis.
“I would argue it’s more powerful than inhibiting something,” he said, noting popular immunotherapy drug pembrolizumab similarly works by boosting a pathway the body uses to fight cancer.
Moving forward, the research team will seek to learn more about p47’s mechanism of action and potential to be developed as a therapeutic. The researchers identified additional genes involved in autophagy that appear to affect metastasis that could become further targets for new treatments.
The gene library Hao custom-developed for this study is also available for other researchers at the Cancer Center and other institutions to use to identify potential targets in other cancers.
Hao began this particular line of research in 2018 and said patience, time, effort and genuine interest in your work are essential for cancer researchers.
Guan said many researchers focus on one protein or gene at a time, but it takes a specific expertise to conduct systematic, impactful research of many genes at one time.
“Mingang’s previous work laid the foundation for this, so this is something very unique that not many labs would be able to perform,” Guan said. “When I recruited him, this was the kind of thing I hoped he could do.”
Impact Lives Here
The University of Cincinnati is leading public urban universities into a new era of innovation and impact. Our faculty, staff and students are saving lives, changing outcomes and bending the future in our city's direction. Next Lives Here.
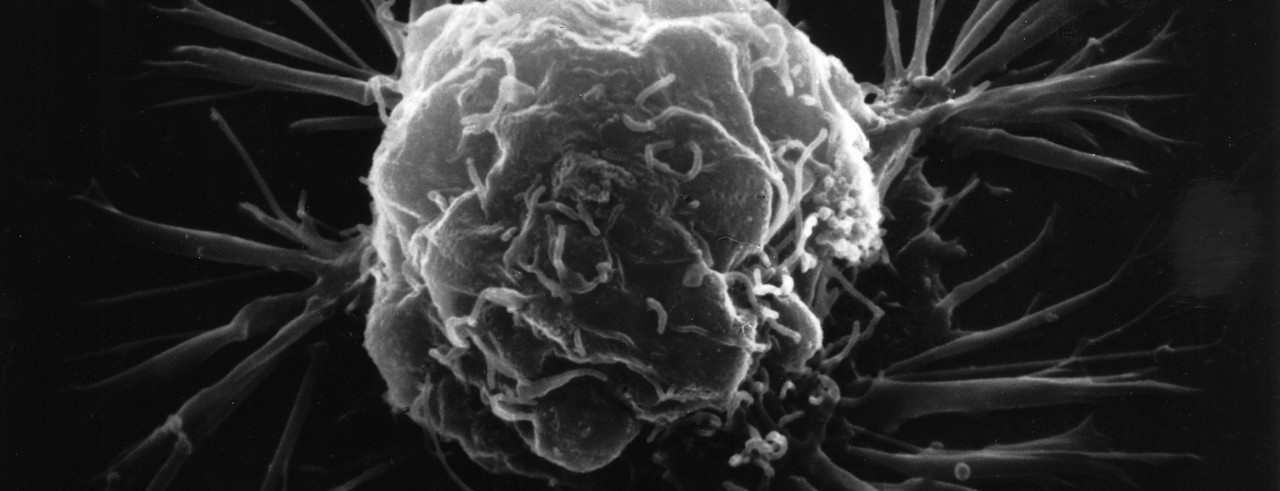
Featured photo of 3D breast cancer cell courtesy of the National Cancer Institute.
This research was funded by the National Institutes of Health (R01 CA211066; R01 HL073394; R01 NS094144). Researchers cite no conflicts of interest.
Related Stories
Study: Synthetic protein potentially improves outcomes for certain subgroups following intracerebral hemorrhage
February 4, 2026
The University of Cincinnati’s Joseph Broderick, MD, presented results from the FASTEST trial at the International Stroke Conference, simultaneously published in The Lancet, that found administering a synthetic protein, recombinant Factor VIIa, can reduce bleeding and potentially improve outcomes for certain patients at the highest risk of continued bleeding following an intracerebral hemorrhage.
Grow and explore in a Fall 2026 Honors Seminar
February 4, 2026
While University Honors Program (UHP) students get priority registration, honors seminars are open to undergraduate students outside the program as well. Try one out for an interdisciplinary, hands-on learning experience like nothing else on campus.
Travel, tattoos & vaccine truths: Clearing up blood donation myths
February 3, 2026
In recent years, the U.S. Food and Drug Administration (FDA) has updated several blood donation deferrals and restrictions. Despite these changes, many myths and misconceptions persist about who can and cannot donate safely.
